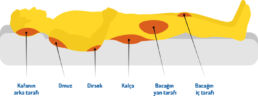
Individuals who are bedridden or receive inpatient treatment for a long time and those who use a wheelchair may develop pressure sores in anatomical areas that face bodily pressure for a long time unless appropriate precautions are taken. Pressure sores often develop in areas of the body where there are bony structures.
External factors
- Infection
- Rubbing/friction on surfaces such as sheets, diapers, clothing
- Force applied when moving the patient
- Humidity
Internal factors
- Poor general condition/perception problems
- Malnutrition
- Age
- Diabetes
- Edema
Bedridden individuals or those who use a wheelchair with urinary incontinence and patients with neurological conditions such as Alzheimer’s and Parkinson’s may encounter being wet rather frequently and that is a source for pressure ulcers. The friction caused by the surface the body comes into contact with also has an effect on the integrity of the skin, accelerating wound development. Pressure sores are often accompanied by disease-causing opportunistic bacteria.
It is important to prevent pressure sores before they develops as it is difficult to treat and care such wounds. At the beginning of a pressure ulcer formation, redness can be seen on the skin exposed to pressure, followed by fluid-filled blisters on the skin surface, darkening of skin color and finally, necrosis. Afterwards, perforation develops with skin ulceration.
Measures to Help Prevent Pressure Sores
Ensure that the skin remains dry and clean.
Take care to frequently change the adult diaper used by your beloved one who has mature skin.
Use hygiene support products that are suitable for personal care and do not contain abrasive agents such as soaps or detergents.
Make sure that the position of your inpatient is changed every 2 hours as recommended by the doctor.
It is also important that your patient is rotated with a minimum risk of friction.
Using an oily moisturizer after cleaning the defecation area may be beneficial for those with fecal incontinence.
In order to avoid irritation of the skin of your inpatient, make sure that the bed sheet is properly smooth and tight.
Try to keep your patient away from any conditions that you know may cause friction.
Have your beloved one who uses a wheelchair lift themselves up every thirty minutes or so by relying on the strength from their arms as recommended by the doctor.
Diarrhea and constipation may also trigger skin irritation. Do not hesitate to get support from the doctor for these complaints.
Upon consulting the doctor, you can apply creams that help soothing and repairing the reddened skin areas caused by friction and irritation.
Adequate support to reduce the load should also be used on the heels of the feet, if under pressure.
You may also try using an airflow bed for your bedridden patient.
Provided that your patient’s condition allows, you can support them for active-passive exercise every eight hours as advised by the doctor.
Source
Saygın H. Basınç Yaralarında Hemşirelik Yönetimi. Erişim tarihi: Kasım 2017.